Patients grateful for call-back second looks after screening mammograms

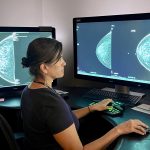
UCHealth/Courtesy photo
If women need any more encouragement to schedule an annual screening mammogram starting at age 40, experts offer some sobering statistics about the aggressive growth of breast cancer for patients in their 40s.
The Society of Breast Imaging, for example, notes that “one in six breast cancers occur in women ages 40-49.”
“Breast cancer is quite common in the age group of 40 to 50,” said Dr. Malaika Thompson, a fellowship-trained breast imaging radiologist in Steamboat Springs. “Starting at 40 is the best way to find cancer at the earliest stage possible when it is the easiest to be treated with the least invasive treatment. The easiest likelihood for cure if you start mammograms at age 40.”
“When younger women, at less than 50 years old, develop breast cancer, it tends to be more aggressive, meaning that it can grow faster,” Thompson explained. “So, unfortunately, the younger that you are when your breast cancer occurs, the more aggressive it tends to be.”
One screening statistic that may soothe possible nerves for patients going in for a standard mammogram at the UCHealth Gloria Gossard Breast Care Center in Steamboat is that nine times out of 10, women complete the annual screening exam with no concerns or call-backs. Their hardest job afterward may be to remember to call the hospital scheduling department to schedule their next annual exam.
Radiologist Thompson has amassed years of experience to be able to compare multiple years of mammogram imaging and notice changes. That is why annual screenings are so important, so that imaging can be compared and changes identified, Thompson said.
“Having all those prior studies (images) is probably the most important thing about mammography,” Thompson said.
The radiologist noted if patients had previous mammograms at different facilities, it is important to let the current breast center staff know where those screenings took place to be requested and compared.

According to the National Cancer Institute, since mammography screening became widespread in the early 1990s, the U.S. breast cancer death rate decreased more than 30% compared to the death rate that was unchanged for the previous 50 years.
“While some people with breast cancer experience symptoms of the disease – most commonly a new lump or mass – mammograms can detect the disease significantly sooner, sometimes up to three years before you or your doctors can feel a mass,” according to the Breast Cancer Research Foundation. “Thirty to 50% of breast cancers that cannot be felt are identified solely by micro-calcifications on a mammogram.”
Thompson said approximately 10% of screening mammography patients at the Steamboat center are asked to come back for a follow-up screening for problem-solving.
“It’s not uncommon for people to get called back in if we see something that needs to have another look,” Thompson said, referring to findings of calcification, asymmetry or a mass. “Across the board, people are always very grateful that we looked harder.”
Radiologist Dr. Malaika Thompson
“Across the board, people are always very grateful that we looked harder.”
That next step of screening would include additional or diagnostic mammogram imaging to investigate specific findings and a possible ultrasound exam, Thompson said. A handheld ultrasound could be performed to check a specific area of concern to further define what was seen on the mammogram. Or sometimes the Automated Breast Ultrasound System, or ABUS, is used for women with very dense breast tissue to see a larger portion of the breast.
The good news is that “80% of call-backs are benign,” said Annie Schwarz, nurse navigator in the Steamboat breast care center.
If a finding is concerning for possible cancer, a patient may need to have a biopsy performed, usually within 10 days. During a biopsy, a tissue specimen is extracted through a core needle device or a vacuum needle device. Those biopsies collect a small amount of suspicious tissue are performed by the radiologist at the breast center using ultrasound-guided imaging and localized numbing.
An incision of a couple of millimeters is made to insert the biopsy needle, so any scarring is minimal. Before and after images are recorded, and specimens are sent to the lab to review under a microscope with results returned in two to three business days.
Thompson said surgical biopsies are much less common now because performing biopsies with the assistance of image guidance and needle extraction devices is most common.
“Everyone uniformly says, ‘that was so much easier than I thought it was going to be,'” Thompson said. “Most of our biopsies are benign.”
“I try to explain to patients is that breasts are very active,” Thompson said of numerous types of breast tissue changes. “They are making a lot of things and doing a lot of normal physiologic processes both pre-menopause and post-menopause. Fibrocystic change is the most common thing; that’s in about 80% of women in general.”
Every patient seen in the Steamboat breast care center is assessed for lifetime risk of developing breast cancer through the Tyrer-Cuzick Risk Assessment Calculator (also available for patients to use online at Magview.com/ibis-risk-calculator) by utilizing personal and family medical history. If that calculator score is 20% or greater for lifetime risk, patients should consider having an MRI screening on their breasts, Thompson advised.
“MRI is the most sensitive tool for identifying breast cancer,” Thompson said.
Nurse Navigator Schwarz provides guidance and answers many concerns related to financial questions or anxiety-driven questions such as timelines and treatments. The nurse navigator can help patients find funding through charitable organizations such as the Bust of Steamboat to cover additional screenings if needed due to insurance gaps.

To reach Suzie Romig, call 970-871-4205 or email sromig@SteamboatPilot.com.

Support Local Journalism

Support Local Journalism
Readers around Steamboat and Routt County make the Steamboat Pilot & Today’s work possible. Your financial contribution supports our efforts to deliver quality, locally relevant journalism.
Now more than ever, your support is critical to help us keep our community informed about the evolving coronavirus pandemic and the impact it is having locally. Every contribution, however large or small, will make a difference.
Each donation will be used exclusively for the development and creation of increased news coverage.